PJ’s story begins with a parent’s worst fear—bullying. Currently in middle school, PJ’s high-functioning Autism left him vulnerable to it. One day, the bullying escalated to a shocking level, resulting in a physical assault that left PJ hospitalized.
Bullying is listed as a type of trauma by The National Child Traumatic Stress Network. Bullying can prevent someone from enjoying a safe, stress-free learning environment. It can lead to stress, anxiety, depression, loneliness/isolation, avoiding school or poor performance in school, self-injury, and even suicidal thoughts and actions. The harmful effects of bullying depend on many things, including the frequency and severity of bullying.

“I wish I could say this was the first time he was bullied. But unfortunately, this was the worst physical time he was bullied,” says PJ’s mom, Kaitlyn.
As PJ underwent intensive outpatient rehab, speech therapy, and occupational therapy, the Ronald McDonald House became PJ and Kaitlyn’s second home. But even with the support of the Nemours Children’s team, he still faced the daunting task of navigating the emotional turmoil of PTSD and anxiety.
“Post-Traumatic Stress Disorder, or PTSD, is a psychological disorder that develops when a child or teen experiences or witnesses a scary or dangerous event,” says Dr. Paul Enlow, a pediatric psychologist on the Behavioral Health team at Nemours Children’s Health, Delaware Valley. “In PJ’s case, this was the physical assault. When people hear about PTSD, they often think of veterans and may have heard about people experiencing flashbacks. However, children and adolescents can also have PTSD. In addition to flashbacks and nightmares about the trauma, people may avoid things that remind them of the traumatic event, feel depressed or anxious, start to think that the world is unsafe, have difficulty sleeping, and parents or caregivers may notice changes in behavior.”
“After a dangerous or scary event, children and teens often experience one or more symptoms of PTSD. Parents can also have PTSD symptoms, even if the traumatic event did not happen to them. For most youth, and parents, these symptoms go away after a few weeks. However, for other people these symptoms do not go away and may require psychotherapy, medication, or a combination of both.”
“When I first started working with PJ, he had just joined our rehab program. He was still using the wheelchair. He was not able to really get around much on his own. From a psychosocial perspective, PJ was very withdrawn, very quiet. In our first session, he spent most of the time with his head down, not really wanting to talk, not wanting to engage. We couldn’t talk much about the trauma that occurred,” says Dr. Enlow.

Cognitive Behavioral Therapy (CBT) is the gold-standard psychological treatment for depression and anxiety. Trauma-Focused CBT is a variation designed specifically for youth with PTSD. “I used TF-CBT with PJ and his family. During therapy, PJ learned strategies to relax his body when he felt anxious and overwhelmed, and how to identify and change unhelpful ways of thinking,” says Dr. Enlow. “Most importantly, TF-CBT involves decreasing avoidance. Understandably, people with PTSD avoid reminders of their trauma or engage in avoidant coping strategies when unwelcome thoughts about the trauma pop into their head. This avoidance strengthens, and perpetuates, PTSD symptoms. A big part of PTSD treatment is helping youth and families ‘face their fears’ in helpful, controlled ways. You might hear psychologists or other therapists call this ‘exposure.’ By engaging in exposure, youth and their families ‘take back’ their life from PTSD and are able to do the things that they enjoy.”
Because the assault occurred in PJ’s neighborhood, home was seen as a dangerous place for PJ, rather than a safe place. “Returning home was a really significant stressor for him,” says Dr. Enlow. “The biggest thing I have seen recently from PJ, is that he made the decision to do things that are hard. He decided, ‘I’m going to stay overnight at my house because it means I get to play with my siblings or spend more time with a friend in the neighborhood.’ That’s a huge accomplishment for PJ.”
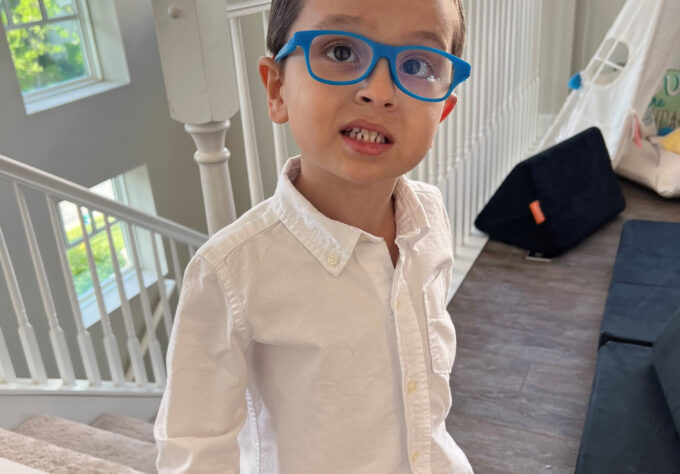
“Now, his personality is out, he loves to joke. He loves to play pranks on his siblings. He loves NASCAR and so he wants to talk about that. He is much more outgoing. He’s much more talkative. I can see PJ rather than the trauma that he was experiencing,” says Dr. Enlow.
In addition to his dedicated care team—Dr. Laura Owens from Physical Medicine and Rehabilitation and Dr. Enlow—the School Program at Nemours Children’s Hospital, Delaware proved to be a sanctuary. Teachers Sharon Miorelli and Colleen O’Shea created a safe space for PJ to learn and grow, providing the stability and support he needed.
“The School Program is an amazing resource,” says Kaitlyn. “Those ladies were there for him for everything.”

“When students come in, we’re very careful to meet them where they are,” says Sharon. “We always get a gauge on how they’re feeling. And sometimes they just don’t feel like working. So, we might just paint or play a game that day. And through those small experiences, it allowed PJ to start to open up and realize that this was a safe space for him.”
As time progressed, Sharon and Colleen were able to incorporate harder academic work into his days. “We’d say to him, ‘Now we’re going to make it a little harder, but you can do it.’ So through being here and working with rehab, he grew and developed confidence. By the time he was done, we could tell that he was ready to just be a teenage boy,” says Sharon.
Sharon and Colleen also recognized the urgency of PJ’s situation and worked to ensure he had the support he needed to get back to school. Colleen worked to secure a 504 Plan for PJ, which ensures that students with disabilities are able to participate in academic and extracurricular activities at school. She also helped him apply to several charter schools; he started this school year at a new school in Delaware.
Over time, PJ’s physical health improved, and he regained his ability to walk unaided. “Physically he is doing so much better. When he first entered the program, he was in a wheelchair, but now he’s up and walking. It’s been amazing watching this transition,” says Kaitlyn. “There were some days where I couldn’t leave his side because the depression was kicking his butt and the PTSD was so intense. But he’s doing amazing now.”

“The whole situation speaks to PJ’s resilience and hard work,” says Sharon. “It’s always amazing to me to watch all the kids that we have in therapy. They put so much time into work and into their recovery. They’ll have two or three therapies a day and then they come to us and do schoolwork, and they’ll work really hard. PJ has not only worked through the physical issues, but also the mental issues with recovering, because of the trauma that he went through. It’s a real testament to his character and the support he had with family and here at the hospital.”
“Kaitlyn is such a fierce advocate for her child; she did every single thing,” says Colleen. “All the T’s were crossed, all the I’s were dotted. She did everything she possibly could for her son.”

PJ’s journey is far from over. Physical therapy and behavioral health counseling with Dr. Enlow will be ongoing as he takes the steps necessary to transition back to normal life.
“My hope for PJ is that he will get out there and make friends, and that he will appreciate school for all the great stuff that it can bring to him,” says Dr. Enlow. “And he’ll just live his life.”
PJ says he wants to share his story to bring awareness to bullying and to speak out against bullying. “He still is trying to work through his fears, but even through the fears, he wants to find a way to help other kids,” says Kaitlyn.
“Along with the bullying awareness, I think mental health awareness goes hand in hand,” says Colleen. “PTSD is invisible for a lot of the time, but it is still affecting PJ and how his life is lived right now. I hope that this reminds people to just be a little bit kinder and give people a little bit more grace, because you can’t always see what they’re going through.”
If you have a child who is being bullied, help is available. Visit Dealing with Bullies (for Kids) or Dealing with Bullying (for Teens) for more information, and the Center for Pediatric Medical Traumatic Distress and The National Child Traumatic Stress Network for resources and information on what to do.
What Leads to Bullying
Oftentimes, bullying is focused on the individuals: the bully and the bullied. However, there are many contextual factors that typically go unnoticed and unaddressed. “There needs to be advocacy at the systems-level to provide better resources for our schools, and community-level initiatives to address violence and poverty,” says Dr. Enlow. “When we get so focused on the bully and the bullied, we forget about all that stuff because we have tunnel vision. And while I’m glad to be able to say, we can give these kids the tools to cope with what he’s been through, it’s not necessarily going to stop the next kid from going through what PJ’s been through.”
“A lot of times we’re focused on treating individuals, but systems are designed to spit out another person who’s going to bully other students. So, it’s it is important to have that systems-level, that health equity approach if we really, really want to address bullying.”